This week for my elective week, I had the wonderful opportunity to work in an outpatient oncology clinic with the outpatient oncology dietitian. These clinics are radiation clinics, so instead of formal appointments every half hour in one location, the dietitian is able to see the patient after their radiation session for as much time as it takes at various radiation oncology sites across Montgomery County. The patient may require a full nutrition counseling session, just ask a few questions or ask for some reading material. It's a great environment where the patients are often really interested in learning about healthy diets to help prevent recurrence of their cancer.
During my week I saw a patient with thymus cancer, which is rare. So for this blog, I'm going to do a quick review of what the thymus does and how it is treated nutritionally.
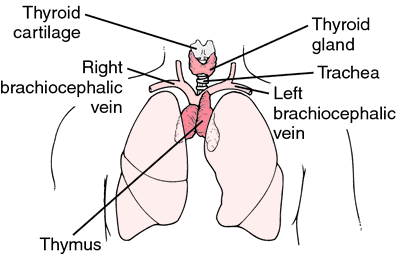
The thymus gland is located in the upper chest, under the breast bone. It's part of the lymphatic system and helps make T-lymphocytes in infancy and childhood, to help fight infection. An interesting note about thymus cancer is that although it is rare, it's most commonly seen in patients with autoimmune diseases like myasthenia gravis, lupus, or rheumatoid arthritis. "Thymic carcinoma" originates in the epithelial cells in the thymus.
Image from thefreedictionary.com
The most common treatment is surgery to remove the malignant tumor, but chemotherapy and radiation are also possible treatments. Nutritionally, it is treated like any other form of lymphoma; focus on getting enough calories and watch for signs of radiation-swallowing issues since the radiation beam may impact the esophagus. In the case of this patient, we focused on a diet full of antioxidant rich fruits and vegetables, lean meats, and whole grains. The patient was extremely interested in healthy eating, and I would say overall a very successful appointment!
Wednesday, June 19, 2013
Sunday, June 16, 2013
A Week in Renal
This week I visited two dialysis centers, one in Oxon Hill, MD and the other in Seat Pleasant, MD. It was an amazing experience and great to see the passion each dietitian put into their work. For patients on dialysis, the process is apart of their daily routine. They must set aside 3 - 5 hours, multiple times per week, where they sit hooked up to a dialysis machine. In order to make the experience more bearable, the dietitians (along with center staff) must get creative.
At the center in Oxon Hill, they award “Phos dollars,” to patients with good phosphorus labs. These dollars are then exchanged for prizes like picture frames, kitchen supplies, and puzzle books. It’s a great incentive for the patients and they really seem to enjoy it. The center in Seat Pleasant holds lab coat decorating contests where the patients are the judges. Most recently, they have musical performances by the staff and play music on special occasions like Valentines Day or Christmas.
Lastly, both facilities have monthly “lobby days,” where the patients can taste test renal-friendly alternatives like almond milk and protein bars.
Overall, I learned that keeping an uplifting and inventive approach to patient care is essential in the outpatient dialysis setting.
Tuesday, June 11, 2013
Reflections of the Final Theme Meal: 1950's Soda Shoppe!
 |
| Windsor Dining Room: Hostess Stand |
Our last rotation of the internship was 6 weeks at Riderwood Senior Living Community. As you may know, this is the rotation where all the interns plan, prepare and execute a theme meal for about 150-200 of the residents. Since we were the last set of interns to come through this particular rotation, we knew we wanted to plan a theme meal so that the 2012-2013 UMD Dietetic interns went out with a bang!
 |
| Maria Tadic, Chef Derrick, Nikki Bolduc and Manager Otto |
We decided to create a theme meal that would really resonate with the residents - something that would remind them of their childhood and growing up in the '40s and 50's. It was important to us to find a theme that they would really enjoy. After some research and chatting up our parents and grandparents we ultimately decided to go with a 1950's Soda Shop with diner-style food. This theme really allowed us to get creative and come up with some really tasty recipes - especially for the desserts!
The final menu included:
- Chicken & Dumpling Soup
- Diner-style Mac & Cheese
- Baked Stuffed Tomatoes
- French Fries
- Cheesy Bacon Meatloaf Sandwiches
- Tuna and Potato Chip Casserole
- Caprese Grilled Cheese Sandwiches
- Root Beer Floats
- Malted Milkshakes
- Banana Splits
We tried to come with as many dishes that were popular in the 1940's and '50's as possible. And from the resident comments, we were right on target! Our menu was super fun to plan, cook and eat too! Something both of us highly recommend for future interns - make your menu and theme fun!
Looking back, I think we hit our goal of exiting Riderwood with a bang! The residents really loved our meal and the theme. Plus we met a lot of great employees and made some wonderful friends while we were here. It was an amazing experience filled with tons of learning and of course, a lot of fun!
Monday, June 10, 2013
What’s the deal with the Dialysis Diet?
Renal disease requires a very specific diet pattern. What happens in kidney failure is that the
kidneys are unable to filter the blood so components that are usually excreted
just build up in the body. This can lead
to dangerous side effects and without dialysis, death. Fortunately, through diet, medications and
dialysis treatment, patients can manage their disease. Here are the biggest things to watch out for,
the 3 P’s:
Protein
- Albumin Goal: ≥4.0
When patients are have renal disease pre-dialysis, they are
on a very low protein diet. All that
changes because the process of dialysis increases their needs to 1.2-1.5g/kg,
up from 0.6-0.8g/kg. That is double!
Because of this, patients need to be encouraged to eat enough protein,
especially from animal sources that are more bio-available compared to
vegetarian sources.
Potassium
– Goal 3.5-5.5
Potassium is a common component of many fruits and
vegetables so what appears to be a healthy diet could be dangerous for a renal
patient. The trouble with potassium is
that it affects muscle contractions in blood vessels, including the heart. A spike can lead to a heart attack, just like
that, so it is critical to keep lab values within an acceptable range.
Phosphorus
– Goal 3.0-5.5
Due to the high demand for protein, patients will consume
more phosphorus than is ideal, but they take ‘binders’ with every meal to soak
up the phosphorus so it is undigested.
One of the major complications associated with uncontrolled Phosphorus
is decline in bone health. High levels
stimulate parathyroid hormone (PTH). In
a body with healthy kidneys, this is a signal to excrete the extra phosphorus. Because it cannot go anywhere, the PTH stays
high and causes damage to the bone, leeching out calcium. In more severe cases, this can lead to
calcification of the soft tissue which is painful and if unchecked can result
in amputation and death.
By adhering to a proper diet, using their medications
correctly and getting all of their dialysis treatments, all of these values can
remain in the healthy ranges. Dialysis
patients may need to work a bit harder, but they can still lead healthy
lives.
Monday, June 3, 2013
Your Clinical Survival Guide
If you’re anything like me, you may find yourself a little intimidated by the prospect of going into your clinical rotation. In my case, it had been a few years since I took MNT, and didn’t have any hospital experience. I’m here to tell you that it’ll all work out! In case you would like to prepare early though, here are a few ideas to help you get a jump start on your clinical rotation.
1. Get the standards of practice and formulary. Most hospitals have a small pocket guide for their recommendations… common equations, protein and calorie recommendations for different populations and disease states. This is extremely helpful when going to see patients! Your formulary is your guide to all the tube feed formulas and supplements available at the hospital along with their macronutrients.
2. Keep a cheat sheet. One of the best things I could have done for my clinical rotation was to get a small notebook you can keep in your lab coat pocket. In this notebook, keep lists of all the important things you may need, like labs, common medications, equations and nutrition care manual recommendations.
3. Know your labs. Most hospitals now are using electronic health records (EHR) and don’t require you to memorize normal lab values, but that doesn’t mean you shouldn’t know them. Get an idea of what the norms should be, and know why they may be off. Why might BUN be high? Why could sodium be low? These are all great things to put in your little book.
4. Know the systems. Remember in school, learning about glycolysis, the function of the kidney, etc? Brush up on them. You don’t need to memorize them, but try to remember the basics on how the functions work. It will better help you understand when something isn’t working right.
And most of all, don’t worry. We all have to start somewhere. No one is an expert right away. Be willing to take a step back and admit you might not know something, and look it up. There are a lot of disease states out there that you may have never heard of. Quickly looking things up can help you find what you need and make the right recommendations.
So now you can relax and be confident that you, too will succeed in clinical!
Subscribe to:
Posts (Atom)